Research Article: 2018 Vol: 21 Issue: 2
Medical Students Opinions on the Inclusion of Non-Traditional Skills in the Curriculum
Chevonne Brady, University of Dundee
Mark Zarb, Robert Gordon University
Abstract
Background:
Up to 50% of foundation year 2 doctors do not proceed directly into speciality training. This change in direction of our profession places increasing demands on an already stretched NHS. In the UK, medical school teaching is understandably focused on the skills students will need as junior doctors. With the shift in career trajectories of these students it is important that medical education evolves with this.
Methods:
Final year medical students have been surveyed regarding their exposure to entrepreneurship and management, as well as their interest in their inclusion in the curriculum.
Results:
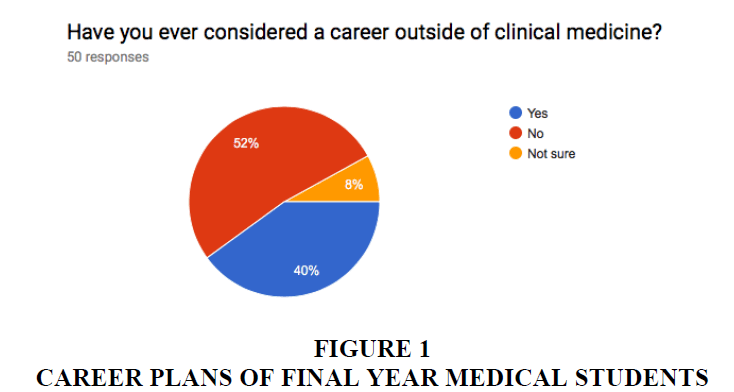
A 10-point survey was completed by final year medical students. No undergraduate students reported having had teaching on entrepreneurship during their degree. Only two students reported having teaching on management skills. 48% reported that they were considering a career outside of clinical medicine, fitting with the findings of the Foundation Programme Career Destination Report.
Conclusion:
Whilst entrepreneurship is now accepted as an important skill for doctors, this is clearly not filtering through to undergraduate medical education. With the help of student feedback, we are now setting-up a pilot programme in entrepreneurship and management for final year students. This will be part of a cross-discipline National teaching programme in entrepreneurship.
Introduction
In the United Kingdom, up to 50% of foundation year 2 doctors do not proceed directly into speciality training (The foundation programme, 2016). This has been a rapid change in the direction of our profession and is placing increasing demands on an already stretched health service (Pollock et al., 1999). The National Health Service (NHS) is a public, government-run enterprise which provides healthcare to all citizens in the UK, free at the point of access. It is frequently held up as a bastion of healthcare and was judged to be the “world’s best healthcare system” by the Commonwealth Fund in 2017 (Schneider et al., 2017). Despite this accolade, the NHS is under significant pressure on a daily basis with growing patient numbers and increasingly complex medical conditions which require treatment. In the midst of this, the number of trainee doctors leaving the NHS is growing on a yearly basis (The foundation programme, 2016; Pollock et al., 1999). The reasons behind this are complex, but poor morale and changes in junior doctor contracts are felt to have significantly contributed (Rimmer, 2016). In the UK, medical school teaching is understandably focused on clinical expertise and improving diagnostic skills which students will need in their jobs as junior doctors. With the shift in career trajectories of these students as well as the increasing number of managers within the health service, it is important that medical education evolves to take this into account. The NHS has recognised this and has developed a fellowship for entrepreneurs within the NHS, with the aim of allowing doctors to develop these skills without leaving their clinical commitments entirely (Young, 2016). These are, however, not widely available as yet and are still in their relative infancy. Medical schools in the UK do not yet appear to have recognised this need to allow doctors to develop in these “non-traditional” roles and these skills are not generally included within the UK medical undergraduate curriculum. Certainly, there is no requirement for their inclusion.
In order to address these two distinct issues of an understaffed health service struggling to retain staff and medical professionals not being able to develop in non-clinical areas as easily as they may like to, this project aims to examine what teaching the next generation of doctors have received on non-traditional skills as well as their opinions on the inclusion of them in the curriculum. Based on this we will then examine how best to integrate these skills into the undergraduate medical curriculum, as well as looking towards collaborating with other centres and departments. As this is a relatively new area being explored in medical education, it is recognised that this cannot be done in isolation and collaboration with other disciplines will be essential to its success.
Methodology
In order to assess what exposure medical students have had to teaching in the areas of management and entrepreneurship a survey was sent to final year medical students at the University of Dundee. Final year students were chosen initially as they will have experienced 4 or 5 years of the curriculum so far and so should have the best idea regarding gaps in their education. A survey was then sent out via email to these students, who were given four weeks to respond. Full ethical approval was granted from the University of Dundee for this data collection process. This survey is shown in appendix. Questions for this survey were based upon two factors: establishing what experience students had already had regarding non-traditional skills education and what their impressions would be in introducing this into the curriculum. In order to engage students in the process of setting up this new teaching programme, they were asked a series of questions on how and when to integrate these teaching sessions into their undergraduate education, which will be used to develop and deliver the new teaching sessions.
The results of the survey will form the basis of a new teaching module which will begin at the University of Dundee. The results of the survey will be used to shape the format of this module, which will initially be stand-alone sessions or “tasters” for the students. In setting up this project, advice was sought from local entrepreneurial organisations including the Centre for Entrepreneurship, Elevator and Business Gateway. The University of Dundee Medical School has been fully involved with this project since its inception.
Results
A short survey was produced and sent out to final year medical students (shown in appendix). This survey has so far been completed by 50 final year medicals students and has yielded some very interesting results. Of note, no medical student reported having any teaching on enterprise or entrepreneurship during their undergraduate education. Two students reported having had formal teaching on management skills. Only 52% of final year students reported that they were not considering a career outside of clinical medicine, fitting with the findings of the Foundation Programme Career Destination Report (The foundation programme, 2016).
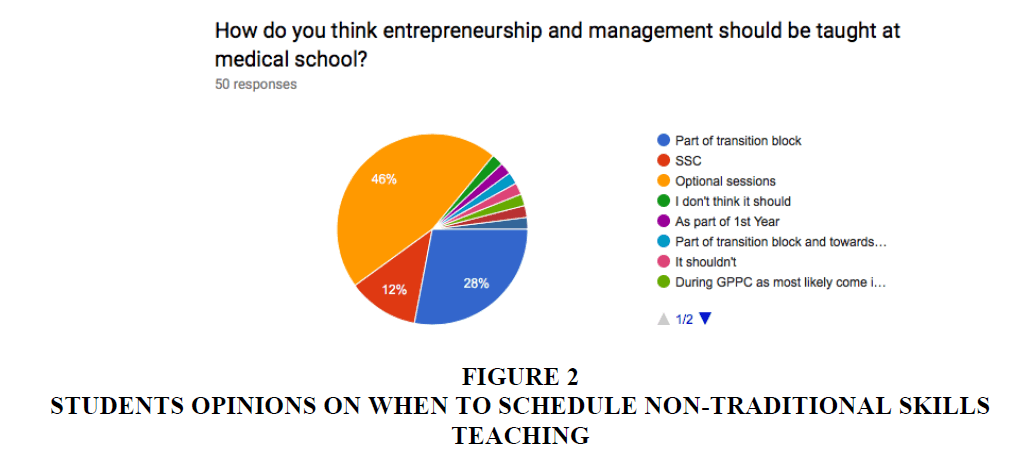
Students were asked where in the curriculum they felt these sessions would best be delivered and results were very varied. 46% of students felt that they should be optional whereas 31.6% of students felt they should be incorporated between the penultimate and final years of medical school. 53.1% of students stating that these would best be delivered at lunchtime and 30.6% felt that they should be after class i.e., in the evening (Figure 1). 62% of students stated that they would consider or definitely attend these sessions.
Students’ free-text responses to the possibility of including these skills in the undergraduate curriculum were highly variable. One student stated “I think it would be beneficial to direct them in the context of integrating them with a NHS career. I am very conscious that any people who go into General practice will especially be required to have a more business mind, focus on business management during GP sessions”, which is very encouraging. Another student interestingly stated that “as long as it is not compulsory, only interested people should attend”. This brings up an interesting challenge in trying to integrate these skills into the undergraduate curriculum. We hope to strike a balance between encouraging interested students to come and develop their pre-existing skills, as well as demonstrate to those who may not immediately understand the usefulness of these skills in their day to day work how important they can be.
For this project, we have sought the input of the School of Computing Science and Digital Media at Robert Gordon University who have set up a similar teaching programme in 2017. With their input, a pilot workshop was run in Dundee in September 2017 funded by the Scottish Informatics and Computer Science Alliance (SICSA). This was attended by over 25 faculty members from many different higher education disciplines across Scotland. During this workshop, educators were invited to present their own experiences of trying to incorporate entrepreneurship and management skills into their curriculum. This aim of this workshop was to determine positive aspects as well as pitfalls that different disciplines may be able to learn from. An introduction to this new project, now known as Skills in Entrepreneurial Education or SEED, was the primary aim of this workshop and was delivered by the authors of this book chapter. Feedback from the day was positive with input from departments across Scotland and across all realms of higher education. The primary outcome of this workshop was to begin a dialogue across the country and across disciplines regarding how to integrate these skills into the curriculum and this was very much achieved.
Discussion
The career pathways for medical students are no longer as straight forward as they once were. Traditionally, medical students graduated from University and proceeded through a structured career path. In previous years, this path was very rarely strayed from, with most doctors graduating from medical school and continuing through training until retirement. At each stage in their career, medical students and doctors have choices to make about their career paths. Following medical school, the vast majority of students proceed into their training as a junior or foundation doctor. The next obvious career break is following foundation training. Each year, the foundation programme publishes data on the destination of trainees. As can be seen in Figure 2, this natural break is the point at which trainee doctors decide upon their speciality and proceed to further training. In 2016, 49.6% of doctors decided not to continue onto the next stage of speciality training (The foundation programme, 2016).
14% of these doctors’ state that they were planning a break from clinical medicine altogether at that time. This is in comparison with 2011, where 71.4% of doctors continued onto further training (Pollock et al., 1999; Young, 2016). As this is a relatively new development in medical careers trajectories, there is limited research into the exact causes, but junior doctors’ morale is known to be very low at this point in time (Pollock et al., 2016; Rimmer, 2016). This presents two problems: An NHS with a depleted workforce and a large number of doctors leaving medicine with limited skill sets outside of patient care. The purpose of this project is to attempt to make plans to combat both of these issues.
Whilst entrepreneurship is now accepted as an important skill for all doctors to be exposed to, this is clearly not filtering through to medical education at the undergraduate level (Young, 2016). The NHS clinical entrepreneurship fellowship is now gaining popularity and allows doctors to combine clinical work with time out of training to pursue their goals, however, it is very much in its infancy (Young, 2016). The aim of this project is partly to allow doctors to develop their ideas with exposure to mentorship and coaching, but also to demonstrate that doctors can be entrepreneurs without compromising their clinical NHS commitments. The aim of this project should be to help prevent the loss of these doctors to the private sector, whilst allowing them to pursue their interests outside clinical practice. In a health service which is experiencing a real recruitment crisis, programs like this will be essential.
A running theme throughout the literature is the fact that doctors are often thrust into management roles based on their clinical experience and not their aptitude or training in management skills (Spehar, Frich & Kjekshus, 2012; O’Kelly, 2017). This may leave the doctors in these roles struggling and with lower job satisfaction than if they were appropriately trained for the job. Many centres have shown that this can be corrected with improvement in both results and job satisfaction.
The NHS is already overstretched by underfunding and chronic understaffing across all areas, but particularly in junior doctor staffing. In 2014-2015, 50% of consultants reported that gaps in rotas existed and 1/5 reported that these were serious enough to significantly affect patient safety (Gulland, 2016). If the trend for junior doctors leaving medicine continues, this is not sustainable for the health service. We therefore believe that non-traditional skills such as entrepreneurship and management should be incorporated within the undergraduate curriculum. These should then be fostered within NHS career pathways with fellowships and additional training to allow doctors to stay within the NHS, whilst building these other interests and skillsets. It must be recognised that these non-traditional skills can bloom within and benefit the NHS. Improved time management skills, awareness of financial responsibility and the ability to self-motivate are all skills which can be learned through enterprising activity and can potentially produce better doctors.
Medical school graduates possess many skills which make them incredibly valuable in the private sector. They are trained in efficient team-working, communication and methodical thinking. They are highly educated, young people who are now looking outside of medicine for future career development. Whilst these students possess many skills, they often know very little of what a career outside of medicine means. We therefore suggest mentoring throughout medical school for these students as well as teaching in key aspects of managerial and entrepreneurial skills as part of the standard medical school curriculum. We believe that the introduction of our SEED programme can both foster these highly-driven students within the NHS and provide them with the essential skills needed to develop their own enterprises.
This survey demonstrates that students are interested in receiving teaching in both management and entrepreneurial skills. The question of how best to integrate them into the curriculum must be guided by their opinions as well as the attempts of other disciplines such as computing science to do this.
Contributors
Miss Chevonne Brady (MBChB (Hons), BMSc (Hons), MRCS) is a core surgical trainee currently training in London, UK with University College London working towards a career in Plastic Surgery. Alongside being a surgical trainee, she is currently pursuing a Master’s Degree in Medical Education with the University of Dundee.
Dr Mark Zarb (FHEA, MBCS) is a course leader and foundation year coordinator within the School of Computing Science and Digital Media at the Robert Gordon University. His main research area is typically computing education, looking at ways to improve the student experience throughout their time in higher education.
Practice Points
• Medical students are interested in the introduction of non-traditional skills into the curriculum
• Faculty development is key in the introduction of this type of teaching programme
• Very little literature is available in the introduction of an entrepreneurship module in undergraduate medical education.
References
- Gulland, A. (2016). Sixty seconds on?. Mind the rota gap. British Medical Journal 353, i2212.
- O?Kelly, S.W. (2007). Management skills need to be systematically learnt. British Medical Journal, 335(7615), 317-318.
- Pollock, A., Dunnigan, M., Gaffney, D., Price, D. & Shaoul, J. (1999). Planning the ?new? NHS: Downsizing for the 21st century. British Medical Journal, 319, 179.
- Rimmer, A. (2016). Junior doctors? low morale is putting patients at risk, royal college of physicians warns. British Medical Journal, 355, i6493.
- Schneider, E., Sarnak, D., Squires, D., Shah, A. & Doty, M. (2017). International comparison reflects flaws and opportunities for better US healthcare. The Commonwealth Fund.
- Spehar, I., Frich, J.C. & Kjekshus, L.E. (2012). Clinicians? experiences of becoming a clinical manager: A qualitative study. BMC Health Services Research, 22(12), 421.
- The Foundation Programme. (2016). Career Destination Report.
- Young, T. (2016). How doctors with entrepreneurial skills will receive NHS help. British Medical Journal, 352.