Research Article: 2021 Vol: 25 Issue: 3S
Factors Affecting Telemedicine Healthcare Services Adoption during Covid-19 Pandemic: A Study In Indian Context
Nishit Kumar Srivastava, ICFAI Business School, IFHE Deemed to be University, Hyderabad
Utkal Khandelwal, Institute of Business Management, GLA University
Trilok Pratap Singh, Madhav Institute of Technology and Science, Gwalior
Anurika Vaish, Indian Institute of Information Technology Allahabad
Citation Information:Srivastava, N.K., Khanadelwal, U., Singh, T.P., & Vaish, A. (2021). Factors affecting telemedicine healthcare services adoption during covid-19 pandemic: a study in Indian context. Academy of Marketing Studies Journal, 25(S3), 1-9.
Abstract
The current study attempts to understand the antecedents to intention to adopt telemedicine healthcare services. In the year 2020 India experienced a tremendous rise in telemedicine service adoption, around a 500 percent increase in teleconsultation was observed. Lockdowns and Covid-19 restrictions acted as a catalyst in telemedicine service adoption. However, the huge population still remains untouched by the benefits of telemedicine healthcare services. In order to understand the drivers of intention to adopt telemedicine healthcare services, a pilot survey is conducted and a research framework is proposed. The following factors are considered for the study: expectation, knowledge, telemedicine experience, prior satisfaction, fear of covid-19 (FC-19), and subjective norms. The proposed framework is then tested using SEM and adequate model fit was observed. The results can be used by policymakers and marketers to enhance the popularity of telemedicine healthcare services among the masses to promote convenience, reach, and healthy living.
Keywords
Telemedicine Healthcare Services, SEM, Telemedicine-Experience, Satisfaction, Fear of Covid-19, Adoption Intention, and Subjective Norms.
Introduction
Continuously increasing Covid-19 infections has overloaded healthcare infrastructure around the globe, limiting access to hospitals. National and/or localised lockdowns have further reduced the mobility of people to hospitals for consultations and medications. Moreover, fear of Covid-19 has led to psychological challenges among the masses leading to panic and discrimination (Pappas et al., 2009; Ahorsu et al., 2020). However, this fear has led people to look for alternative channels of healthcare services and has mobilised telemedicine healthcare services (THS) adoption which was in nascent stage in most of the countries including India. Fear of Covid-19 has acted as a catalyst in impacting behavioural intention of people towards THS adoption. Telemedicine can be seen as a canopy incorporating any medical activity with an element of distance (Wootton, 2001). Telemedicine services use communication technologies in providing healthcare to the participants/patients separated by distance (Donner et al., 2018; Zobair et al., 2018). Almost two third of Indian population resides in rural areas and telemedicine can act as a boon for them providing access to quality healthcare.
According to a report published in Indian express in June 2020, India observed a 500 per cent rise in healthcare teleconsultations where, 80 per cent of the users were first time users (Indian Express, 2020). Further, it was reported that around 5 crore Indians during the period of March to May 2020 accessed healthcare services online (Indian Express, 2020). Further, according to a report published by Statista in October 2020 telemedicine market is expected to increase to 5410 million USD which is almost 5-fold increase compared to current expenditure (Statista, 2020).
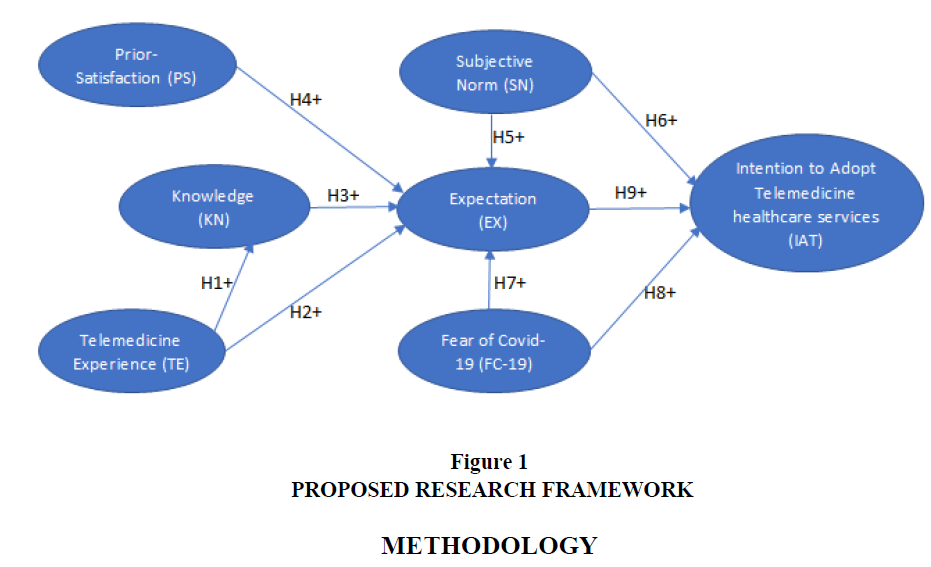
Telemedicine has tremendous advantage which can cater to the healthcare needs/requirements of the huge population of India. So, it becomes utmost important to study the factors affecting the behavioural intention of people to adopt telemedicine. Initially a pilot study is conducted to understand the factors. Based on the pilot study, the proposed framework considers the following factors: expectation (EX), knowledge (KN), Telemedicine-experience (TE), prior-satisfaction (PS), fear of covid-19 (FC-19) and subjective norms (SN) and their impact on intention to adopt telemedicine healthcare services (IAT).
Theoretical Framework and Hypotheses
Telemedicine-Experience (TE)
Experience of consumers play a key role in behavioural research (Hoch and Deighton, 1989). Consumers learn and adapt from their experiences of product or service usage creating a pool of knowledge which leads to formation of expectation triggering future behavioural intention to adopt (Zobair et al., 2018).
H1: TE positively influences users’ KN of telemedicine healthcare service.
H2: TE positively influences users’ EX of telemedicine healthcare service adoption.
Knowledge (KN)
Knowledge refers to familiarity with the product/service triggering learning, exploration and continued usage (Zobair et al., 2018; Webb, 2000). High level of familiarity refers to prior knowledge and experience which in turn leads to firmly rooted beliefs and expectations about THS (Douglass, 2000).
H3: KN positively influences users’ EX of telemedicine healthcare service adoption.
Prior-Satisfaction (PS)
Prior-satisfaction is an individual past experience with a service (Lankton and Wilson, 2007). Favourable prior-experience leads to higher level of satisfaction (Shankar et al., 2003). Satisfaction with the service further contributes to formation of expectations with the THS (Lankton and Wilson, 2007).
H4: PS with the telemedicine service positively influences EX of telemedicine healthcare service adoption.
Subjective Norm (SN)
Subjective norm relates to societal approval of a behaviour (Lai, 2007). Societal setup of friends, relatives and acquaintances impacts an individual behaviour to perform a particular task (Zobair, 2019). Society with prior satisfaction of a service is most likely to positively impact the expectation of an individual to adopt telemedicine healthcare services.
H5: SN positively influences users’ EX of telemedicine healthcare service.
H6: SN positively influences users’ IAT.
Fear of Covid-19 (FC-19)
Fear is a negative force, however, on several occasions it has acted as motivation to do right things. Algie and Rossiter in 2010 found that fear of punishment motivates vehicle owners to follow traffic rules leading to better road safety (Algie and Rossiter, 2010). Ahorsu along with is team of researchers in 2020 presented a fear of Covid-19 scale to counter spread of Covid-19 cases (Ahorshu et al., 2020). Fear as a negative emotion can play a significant role in reshaping expectations and triggering adoption behaviour.
H7: FC-19 positively influences users’ EX of THS.
H8: FC-19 positively influences users’ IAT.
Expectation (EX)
Expectations have been observed to inspire behaviour. It can be defined as the pre-exposed beliefs of an individual towards a product or a service (Zeithamal et al., 1993). Expectations can also be defined as the probability of occurrence of an event based on consumers perception (Oliver, 1981). It acts as a foundation for attitude formation impacting to level of satisfaction decisions (Oliver, 1980). Since, IOT enabled technologies are more compliant and standardized and hence are better equipped and capable to satisfy an individual’s expectations. Hence, from the above discussion it can be hypothesized that expectations positively influence IAT telemedicine healthcare services.
H9: EX positively influences ITA telemedicine healthcare services.
Based on the above developed hypotheses, the proposed conceptual framework is as shown in Figure 1.
Methodology
Sampling
For the current study, sample comprised of volunteers from four major cities of India: Hyderabad, Chennai, Delhi and Mumbai. Due to financial constraints convenience sampling method was adopted and questionnaire was administered through emails. Participants having prior experience of using telemedicine healthcare services were considered for the study. Total of 485 responses were received of which 467 were complete and usable.
Measures
Scale adopted for the study was seven-point Likert scale varying from 7=strongly agree to 1=strongly disagree. Validated and Standardized scales from past researches were adapted for this research. Three items of knowledge, four items of telemedicine experience, three items of prior satisfaction and four items of expectations were adapted from past researches (Lankton and Wilson, 2007; Zobair, 2019). Three items of subjective norm and three items of intention to used were adapted from the work of Cobelli, Cassia and Burro (Cobelli et al., 2021). Fiinally, seven items of fear of covid 19 were adopted from the research work of Ahorsu and authors (Ahorsu et al., 2020).
Results
Normality and Common Method Bias
The model comprised of 27 observed and 6 latent variables. To assess the common method bias Herman’s single factor test was conducted. The variance explained by the single factor came out to be less than 50 per cent, hence establishing that the data free from common method bias (Chauhan et al., 2019).
Mahalanobis distance was calculated to assess the normality of the data, 93.7 per cent of the values were lying between two sigma levels and hence it can be said that the data is normally distributed (Chatterjee et al., 2019).
Reliability and Validity
Reliability and validity of the data was established through confirmatory factor analysis. Construct reliability was established using composite reliability and Chronbach’s alpha was used to establish inter item reliability. The value of the Chronbach’s alpha and composite reliability were above the threshold limit of 0.7 and hence construct reliability and inter-item reliability is confirmed (Table 1) (Srivastava et al., 2018). For convergent validity, factor loadings and average variance extracted was analysed which were above the limit of 0.6 and 0.5 and hence convergent validity is established as shown in Table 1 (Hair et al., 1998). Further, discriminant validity is established as square root of AVE is more than the correlation among constructs (Table 2) (Fornell & Lacker, 1981).
| Table 1 Cross-Loading of Items | ||||
| Item Code | Factor Loading | Composite Reliability | Cronbach’s Alpha | AVE |
| TE1 | 0.930 | 0.967 | 0.962 | 0.845 |
| TE2 | 0.959 | |||
| TE 3 | 0.906 | |||
| TE 4 | 0.880 | |||
| KN1 | 0.862 | 0.944 | 0.922 | 0.849 |
| KN2 | 0.907 | |||
| KN3 | 0.824 | |||
| PS1 | 0.805 | 0.887 | 0.872 | 0.739 |
| PS2 | 0.896 | |||
| PS3 | 0.876 | |||
| EX1 | 0.906 | 0.884 | 0.794 | 0.726 |
| EX2 | 0.880 | |||
| EX3 | 0.865 | |||
| EX4 | 0.893 | |||
| SN1 | 0.951 | 0.965 | 0.962 | 0.893 |
| SN2 | 0.946 | |||
| SN3 | 0.938 | |||
| FC-19-1 | 0.840 | 0.953 | 0.934 | 0.782 |
| FC-19-2 | 0.932 | |||
| FC-19-3 | 0.824 | |||
| FC-19-4 | 0.865 | |||
| FC-19-5 | 0.920 | |||
| FC-19-6 | 0.859 | |||
| FC-19-7 | 0.865 | |||
| ITU1 | 0.874 | 0.913 | 0.896 | 0.724 |
| ITU2 | 0.820 | |||
| ITU3 | 0.792 | |||
| Table 2 Measurement Model Results | |||||||
| Constructs | TE | KN | PS | EX | SN | FC | ITU |
| TE | 0.919 | ||||||
| KN | 0.665** | 0.921 | |||||
| PS | 0.533** | 0.564** | 0.855 | ||||
| EX | 0.582* | 0.524** | 0.522* | 0.852 | |||
| SN | 0.564** | 0.672** | 0.584** | 0.656** | 0.945 | ||
| FC | 0.523* | 0.669** | 0.541** | 0.550** | 0.734** | 0.884 | |
| ITU | 0.537* | 0.074 | 0.656** | 0.665** | 0.551** | 0.734** | 0.850 |
Measurement Model and Hypothesis Testing
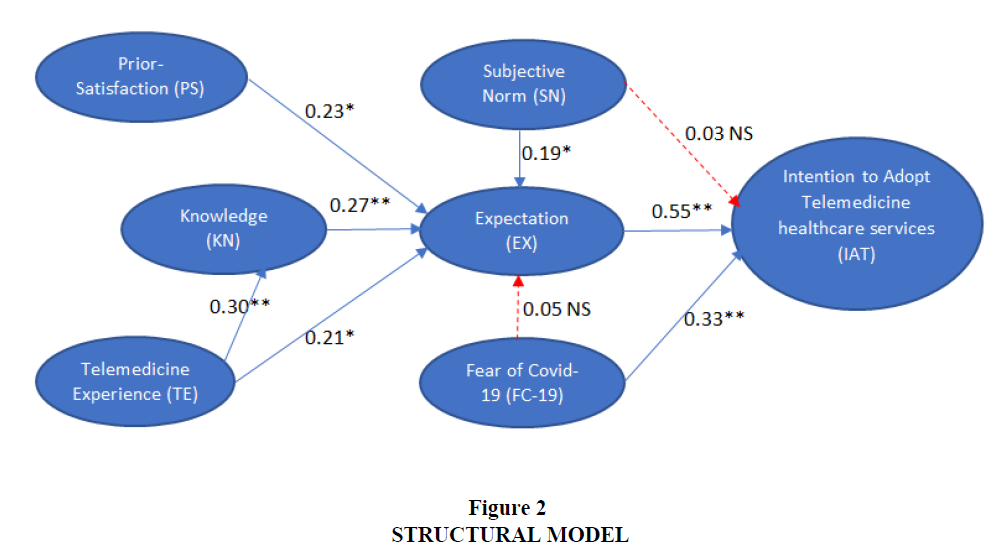
SEM was conducted to evaluate the measurement model; AMOS 20 version was used. Model fit indices presented an adequate model fit: χ2 = 384.592, χ2/df = 2.371, GFI = 0.911 (acceptable >0.9 (Bagozzi & Yi, 1988)), TLI = 0.912 (acceptable >0.9 (Bagozzi & Yi, 1988)), CFI = 0.919 (acceptable >0.9 (Bentler, 1989; Bentler, 1990)), IFI = 0.928 (acceptable >0.9 (Chauhan et al., 2019), RMSEA = 0.06 (acceptable <0.08 (Hair et al., 1998)). The structural model is shown in figure 2.
The hypotheses test results are as shown in Table 3. All the hypotheses except H6 and H7 are significant at 0.05 level of significance. H1, H3, H8 and H9 are significant at 0.001 significance level while H2, H4 and H5 are significant at 0.01 significance level.
| Table 3 Path Relationship of SEM | |||
| Hypothesis | Structural path | Standardized coefficient (p-value) | Relationship |
| H1 | TE -> KN | 0.30** | Supported |
| H2 | TE -> EX | 0.21* | Supported |
| H3 | KN -> EX | 0.27** | Supported |
| H4 | PS -> EX | 0.23* | Supported |
| H5 | SN -> EX | 0.19* | Supported |
| H6 | SN -> IAT | 0.03 NS | Not-Supported |
| H7 | FC-19 -> EX | 0.05 NS | Not-Supported |
| H8 | FC-19 -> IAT | 0.33** | Supported |
| H9 | EX -> IAT | 0.55** | Supported |
| Note: *p<0.01**p<0.001; NS = Not-significant | |||
Discussion and Conclusion
The current study attempts to understand the factors triggering the adoption intention of telemedicine healthcare services in India. The model test results support the proposed framework and all the factors are observed to posit a significant direct or indirect impact on IAT. Expectation is observed to posit a significant positive direct impact on IAT with coefficient value of 0.55, the standardized and compliant nature of communication technology results in greater satisfaction of expectations leading to high IAT (Oliver, 1980). FC-19 is observed to have a direct significant positive impact on IAT with coefficient value of 0.33, FC-19 is a motivation derived out of fear to comply with covid-19 safety norms and yet avail the necessary services through alternate channels (Ahorsu et al., 2020). PS, KN, PS and SN are another important factor which are observed to posit a significant positive impact on EX and play a key role in formation of expectation. SN is observed to have a positive impact on IAT but is not significant at 0.05 level of significance however SN play an important role in formation of expectation and hence posit an impact on IAT through EX. FC-19 is observed to posit a positive impact on EX but is not significant at 0.05 level of significance.
This study may provide policy makers and marketers with crucial insights to understand the behavior of the people and market/promote the services to shape the adoption intention of telemedicine healthcare services.
Appendix 1
Telemedicine-Experience (TE)
TE1: Better access to telemedicine healthcare services is an important experience to me.
TE2: I am ready to wait for longer duration to get specialist services in telemedicine healthcare system.
TE3: The specialized treatments inspire me to used telemedicine healthcare services.
TE4: Using technology-based telemedicine healthcare services is easy for me.
Knowledge (KN)
KN1: I have adequate knowledge about how to use telemedicine healthcare services.
KN2: I have adequate knowledge about how to get health related support through telemedicine healthcare services.
KN3: I think health-related knowledge is important and should never be neglected.
Prior-Satisfaction (PS)
PS1: Telemedicine healthcare services have satisfied my needs.
PS2: Telemedicine healthcare services provides timely responses from specialised hospitals.
PS3: Telemedicine healthcare services improve communication between my specialist physician and me.
Expectation (EX)
EX1: I expect timely responses from healthcare specialists in telemedicine healthcare service system.
EX2: I expect telemedicine healthcare services to enhance my communication with healthcare experts.
EX3: I expect better healthcare access by using telemedicine healthcare services.
EX4: I expect better quality of care by using telemedicine healthcare services.
Subjective Norm (SN)
SN1: People who influence my behavior think that I should use telemedicine healthcare services.
SN2: People who are important to me think that I should use telemedicine healthcare services.
SN3: People whose opinion matters to me think that I should use telemedicine healthcare services.
Fear of Covid-19 (FC-19)
FC-19-1: My fear of coronavirus-19 motivates me to use telemedicine healthcare services.
FC-19-2. I am uncomfortable to think about coronavirus-19 and hence telemedicine healthcare services are a better choice.
FC-19-3. My hands become clammy when I think about coronavirus-19 and hence telemedicine healthcare services are a better choice for me.
FC-19-4. My fear of losing my life because of coronavirus-19 force me to use telemedicine healthcare services.
FC-19-5. When watching news and stories about coronavirus-19 on social media, I become nervous or anxious and hence using telemedicine healthcare services are a better choice.
FC-19-6. I cannot sleep because I’m worrying about getting coronavirus-19 and hence to avoid social contact telemedicine healthcare services are a better choice.
FC-19-7. My heart races or palpitates when I think about getting coronavirus-19 and hence to avoid physical presence in hospital for care services telemedicine healthcare services are a better choice.
Intention to Use (ITU)
ITU1: I intend to use telemedicine healthcare services in future.
ITU2: I predict I would use telemedicine healthcare services more frequently in future.
ITU3: I plan to use telemedicine healthcare service in future.
References
- Ahorsu, D.K., Lin, C.Y., Imani, V., Saffari, M., Griffiths, M.D. and Pakpour, A.H. (2020). The fear of Covid-19 scale: Development and initial validation. International Journal of Mental Health and Addiction.
- Algie, J. & Rossiter, J.R. (2010). Fear patterns: A new approach to designing road safety advertisements. Journal of Prevention and Intervention in the Community. 38(4). Pp. 264-279.
- Bagozzi, R.P., & Yi, Y. (1988). On the evaluation of structural equation models. Journal of the Academy of Marketing Science. 16(1). 74-94.
- Bentler, P.M. (1989). EQS Structural Equations Program Manual. BMDP Statistical Software, Los Angeles, CA.
- Bentler, P.M. (1990). Comparative fit indexes in structural models. Psychological Bulletin. 107(2). 238-246.
- Chatterjee, N., Das, N. and Srivastava, N.K. (2019). A structural model assessing key factors affecting women’s entrepreneurial success: Evidence from India. Journal of Entrepreneurship in Emerging Economies. 11(1). 122-151.
- Chauhan, V., Yadav, R. & Choudhary, V. (2019). Analyzing the impact of consumer innovativeness and perceived risk in internet banking adoption, Internet banking adoption. 37(1). 323- 339.
- Cobelli, N., Cassia, F. and Burro, R. (2021). Factors affecting the choices of adoption/non-adoption of future technologies during coronavirus pandemic. Technological Forecasting & Social Change, Vol 169, 120814, pp.1-7
- Donner, C.F., Raskin, J., ZuWallack, R., Nici, L., Ambrosino, N., Balbi, B., Effing, T., (2018).
- Douglass, C.W., Sheets, C.G., (2000). Patients ‘expectations for oral health care in the 21st century. J Am Dent Assoc. 131, 3S–7S.
- Fornell, C., & Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. Journal of Marketing Research, 18(1), 39–50.
- Hair, J.F., Anderson, R.E., Tatham, R.L. and Black, W.C. (1998). Multivariate Data Analysis. 7th ed., Pearson Prentice Hall. New York. NY.
- Hoch, S.J., Deighton, J., (1989). Managing what consumers learn from experience. J. Mark. 1–20.
- Incorporating Telemedicine into the Integrated Care of the COPD Patient A Summary of an Interdisciplinary Workshop Held in Stresa, Italy, 7–8 September, 2017. Respiratory Medicine.
- Indian Express (2020), 500% rise in healthcare tele consultation in India, 80% are first time users: Report. https://indianexpress.com/article/lifestyle/health/500-increase-in-healthcare-teleconsultation-in-india-80-are-first-time-users-report-6483212/ (Accessed on 24th May 2021).
- Lai, P., (2017). The literature review of technology adoption models and theories for the novelty technology. JISTEM-J. of Info. Syst. and Tech. Manag. 14 (1), 21–38.
- Lankton, N.K., Wilson, E.V., (2007). Factors influencing expectations of e-health services within a direct-effects model of user satisfaction. e Serv. J. 5 (2), 85–112.
- Oliver, R.L. (1980). A cognitive model of the antecedents and consequences of satisfaction decisions. J. Mark. Res. 460–469.
- Oliver, R.L., (1981). Measurement and evaluation of satisfaction processes in retail settings. J Retail. 57 (3), 25–48.
- Pappas, G., Kiriaze, I.J., Giannakis, P., & Falagas, M.E. (2009). Psychosocial consequences of infectious diseases. Clinical Microbiology and Infection, 15(8), 743–747.
- Shankar, V., Smith, A.K., Rangaswamy, A., (2003). Customer satisfaction and loyalty in online and offline environments. Int. J. Res. Mark. 20 (2), 153–175
- Srivastava, N.K., Mondal, S., Chatterjee, N. and Parihar, S. (2018). Identifying critical factors for various maintenance policies: a study on Indian manufacturing sector.
- International Journal of Productivity and Quality Management (IJPQM). 25(1). 41-63.
- Statista (2020). Telemedicine market size in India from 2010 to 2019, with estimates until 2025. https://www.statista.com/statistics/1174720/india-telemedicine-market-size/ (Accessed on 24th May 2021).
- Webb, D. (2000). Understanding customer role and its importance in the formation of service quality expectations. Serv. Ind. J. 20 (1). 1–21.
- Wootton, R., 2001. Telemedicine. BMJ 323 (7312), 557–560.
- Zeithaml, V.A., Berry, L.L., Parasuraman, A., (1993). The nature and determinants of customer expectations of service. J Acad Mark Sci 21 (1), 1–12.
- Zobair, K.M., Sanzogni, L., & Sandhu, K. (2019). Expectations of telemedicine health service adoption in rural Bangladesh. Social science & medicine. 238. 1-10.