Review Article: 2022 Vol: 26 Issue: 4
Charting Organizational Factors that Influence Patient Experience In Indian Healthcare: A Netnographic Approach
Harish B Suri, National Institute of Industrial Engineering
Sanjeev Verma, National Institute of Industrial Engineering
Citation Information: Suri, H.B., Verma, S. (2022). Charting organizational factors that influence patient experience in Indian healthcare: Anetnographic approach. Academy of Marketing Studies Journal, 26(4),1-16.
Abstract
Background- Is it the hospital brand or the quality of infrastructure or patient care, which facilitates a decision when a patient needs to be taken into a hospital. Experience is bound to take place irrespective of the fact whether the person is going as an Outpatient or Inpatient or as a mere companion. Experience of the patient is emerging as one of the key differentiators while choosing or recommending a hospital unless it is an absolute emergency.
Purpose- The list of determinants that influence patient care can broadly be classified as Organizational or Personal or Marketing mix. The purpose of this study is to understand patient’s experience during their visit to the hospitals, qualify the organizational constructs, and then list out the determinants which can be ranked in terms of their impact.
Methodology- The study has been carried out using Netnography (Ethnography on Internet), Kozinet’s 5 step research process and manual coding. In this study, outcomes have been analyzed to identify determinants in Indian context and gauge contributions to patient experience. Results- The emergent themes pointed at the possibility of grouping variables like Systems and Processes, Transparency and Tangibles into one set which creates Value from an organizational perspective. The analysis of discussion threads (DTs) combined with findings of literature review provided an expanded view of key factors responsible for patient’s experience.
Conclusion and Implications- By focusing on Organizational Value creation and its dimensions, it is possible to pave way for practitioners to ensure positive experience for the patients. By reckoning the priority accorded by patients to identified dimensions, generating good experience is possible for promoters as well as professionals managing the hospitals. The findings show that despite low penetration of internet, Indian consumers (patients) are vociferous in articulating their experiences on social media and demanding appropriate attention with services commensurate to the money spent.
Keywords
Patient Experience, Patient Engagement, Patient Care, Hospital Facilities, Healthcare Infrastructure.
Introduction
Studies have been done to understand Patient Experience-PX in a healthcare environment (Becker & Steinwald, 1981; Stein et al., 2005; Sofaer & Firminger, 2005; Vogus & Mc Clelland, 2016; Ferrand et al., 2016; Zakkar, 2019; Gualandi et al., 2019,). Coverage ranged from a solo doctor’s clinic to a big hospital with battery of doctors. Hospitals in western world have started to focus on Patient Experience (PX) and created a dedicated function to strategize, focus, monitor, compute and evaluate the overall PX. Institutions like Mayo clinic and few others are continually improving their patient experience (PX) by data-driven patient-centered initiatives (Iyer et al., 2018). Few hospitals now offer dissatisfied patients partial refunds, reasoning that the long-run value of the feedback received from these patients will outweigh the short-term loss in revenue (Ferrand et al., 2016; Ellison, 2015).
Need for Study
In the healthcare industry, it has been observed that hospitals which focus on patients first have greater patient satisfaction, enjoy better market share and healthy profits (Studer, 2003). Such hospitals also face fewer litigations w.r.t. malpractices, consumerisms etc. Big consulting companies like Accenture, McKinsey, E&Y, Gartner, and KPMG et al, have formed healthcare verticals within their organizations that focus upon and provide solutions to address patient’s experience for effective healthcare management.
In India, researchers focused on dimensions, factors, and other relevant constructs to understand patient satisfaction in healthcare industry (Duggirala et al, 2008; Naidu, 2009; Padma et al., 2010; Chahal & Mehta, 2010; Meesala & Paul, 2018) but no study on patient experience as a precursor to patient satisfaction could be found.
The demand for addressing the needs of a patient and achieving satisfaction by improving the quality of processes was recognized by academicians as well as practitioners (Vogus & McClelland, 2016) and surveys were conducted (Quigley et al., 2015; Padma & Wagenseil, 2016) to capture the dimensions contributing to patient satisfaction. Perceptions of a patient in a healthcare service scape (Sag et al., 2018) has also been methodically reviewed. The healthcare institutions are a complex environment (Duggirala et al., 2008) and the patient comes in direct contact with people, processes, and other aspects of the hospital.
With growing privatization of Indian healthcare sector and the need to stay competitive, it is becoming imperative for the healthcare providers in India to comprehend the dynamics in orchestrating patient’s experience (Deloitte report, 2017). Hence, the need to understand the organizational value creation and its impact on patient’s experience is gaining importance.
We adopted a qualitative technique of collating the views expressed on websites which aggregate opinions given out by patients. This article, using Netnography (Internet+Ethnography), attempts to gather patient insights in understanding the value creation by an organization and its influence in mapping of patient’s experience. The results can be used by academicians and practitioners in gaining critical insights with respect to healthcare systems. The author’s review highlights and underscores how prioritization of the dimensions can help future researchers in designing a high functioning and robust healthcare delivery systems in India and other parts of the world.
Rest of this paper describes the literature review, the research methodology with underlying reasons, findings, discussions, and outcomes. Finally, the researcher also talks about limitations of this study and future scope.
Literature Review
Definition of Patient Experience
The AHRQ (2017) in the USA provides the following definition for patient experience: Patient experience encompasses the range of interactions that patients have with the health care system, including their care from health plans, and from doctors, nurses, and staff in hospitals, physician practices, and other health care facilities. Patient experience often results in perceptions and responses, which are usually affected by the extent of conformation between the expectations of the patient about the different aspects of healthcare and the actual reality of those aspects (Press, 2006; Zakkar, 2019).
Antecedents of Patient Experience
Berry & Carbone (2007) talk about how patient experience strategies deal with practical quality of delivering the services, proficiency of the organization (Systems and Processes), provision of tangibles like good facilities and conducive environment clubbed with cultural factors like trustworthiness. In the same breath, the study also lists out consistent training, efficient interactions between patients and service providers as vital ingredients for generating good customer experience.
Need of Patient Experience Strategies in Healthcare
Creating and delivering superior patient experience in the healthcare industry is gaining enormous attention (Worlu et al., 2016). The dynamic changes in patient’s behavior and commensurate demand for delivery of services is compelling the healthcare organizations to sharpen, strengthen and develop their patient experience strategies.
Factors Considered by Patients to Evaluate Hospital
Patients use more than 500 criteria to evaluate the hospital’s quality while gaining experience (Zifko-Baliga & Krampf, 1997). In the extant study by this researcher, the focus was mainly on organizational level attributes listed out by other scholars.
The following (Table 1) attempts to summarize the dimensions associated with value creation done by the organization. Previous scholars have listed, studied, evaluated patient satisfaction in healthcare institutions. We have considered the research papers published by scholars in the recent past (After 2015) who have reiterated and captured the dimensions specified in the past.
| Table 1 Dimensions (Organizational) Considered by Research Scholars to Study Patient Satisfaction | |||
| S. No | Organizational level Dimensions Studied | Year | Scholars/Agency |
| 1 | Infrastructure (Tangibles), Trustworthiness (Transparency), Administrative processes (system), Clinical care (process) | 2015 | Panchapkesan et al |
| 2 | Physical maintenance (Tangibles), Operational activities (system), prompt attention given by nurses and physicians (process), Trustworthiness | 2016 | Shabbir & Malik, 2016 |
| 3 | Delivery of Services (process), Trustworthiness (transparency), Physical environment, safety of facilities | 2016 | Worlu et al., 2016 |
| 4 | Cultural Competency, Service Delivery (process), time and temporal conditions | 2016 | Vogus & McLelland,2016 |
| 5 | Admission Process, Discharge Process, Filling multiple forms, Room allocation, Medicines stock, choice of non-medical support – All pertaining to System Approach | 2017 | Report by Deloitte |
| 6 | Safety, Clean premises, Delivery of Processes, Approach to processes like teamwork, Supervisory support | 2017 | Ferrand et al., 2016 |
| 7 | Physical Infra, Service scape, Functionality, Ambience | 2018 | Sag et al., 2018 |
| 8 | Wait time, Pharma Automation & Management, Process efficiency, Tele-medicine | 2018 | Alam S et al., 2018 |
| 9 | Admission/Discharge Process improvements, (System), Physical layout, Clinical quality of care (Outcome), Process Orientation, Patient flow | 2019 | Gualandi et al., 2019 |
| 10 | Healthcare facilities, Clinical processes delivery, addressing non-health needs | 2019 | Zakkar, 2019 |
| 11 | Service experience, Service provider professionalism, Mindfulness-Organizational level | 2021 | Boakye et al., 2021 |
Value Creation through Organization Factors
The extant literature pointed at factors encompassing multitude of dimensions besides organizational factors viz. personal factors, and marketing factors. Each cluster of dimensional aspect has its own significance. Present study aims to highlight the organizational factors contributing to patient’s experience. The researcher has collated the essence of factors like System & Processes, Transparency, Tangibles etc. and their respective impact on patient experience.
System and Processes impacting Patient Experience
Hospitals that fail to understand the importance and criticality of delivering patient satisfaction may be facing the chances of extinction (Andaleeb, 1998). Service delivery processes constitute one of the hedonistic contributors of patient experience and an important stimulus that contributes to value creation for the patients (Harris et al., 2001; Boakye et al., 2021). Any patient undergoing treatment at a healthcare institution, must feel assured about being in capable hands. (Parasuraman et al., 1985). The competence in delivering the service and adhering to the processes contribute to patient assurance. Hospitals in USA that had good infrastructure, pleasantness of surroundings, hassle free practices during admission & discharge, well equipped laboratories and diagnostic equipment, contributed to overall patient satisfaction (Otani et al., 2004).
Brady & Cronin (2001) highlighted importance of systems and processes by stating that factors like waiting time, admission processes, discharge formalities etc. should be reckoned as important dimensions in the hierarchical model to measure overall satisfaction (Le et al., 2006).
Hence, System and processes is one of the main dimensions specified and considered.
Tangibles impacting patient experience: Vandamme & Leunis (1993) talked about Tangibles and its value creation being important factors of patient satisfaction. Past researchers in India have emphasized that under the gamut of organizational factors, tangibles are a significant influencer of the patient satisfaction (Chahal et al., 2004; Rohini & Mahadevappa, 2006; Naidu, 2009).
Rao et al (2006), developed a scale to measure perceptions of in-patients as well as out-patients, found that factors like clinical infrastructure, medicine availability etc. were important dimensions to measure patient satisfaction. Physical environment, design, ambient conditions were reckoned to be important dimensions while measuring overall satisfaction (Brady & Cronin, 2001). A study on hospitals in Bangalore, India, by applying SERVQUAL framework, revealed that a gap existed between perceptions of patients and management of the healthcare providers (Rohini & Mahadevappa, 2006).
Hence, Tangibles is one of the main dimensions specified and considered.
Transparency impacting patient experience: Ethics is the center-point of any healthcare system (Seedhouse, 2008). It is anticipated that every heath care institution would embrace certain level of transparency while delivering and discharging their professional services. Healthcare also comprises high degree of morality (Worlu et al., 2016) and it is expected that everyone in the healthcare arena should adhere to best of their professional capabilities in the chosen area of expertise. It is also prescribed that organization must strive to earn respect as a trustworthy entity. Focus on the patient is directly linked to the drive for transparency and creating greater accountability in health care (Sofaer & Firminger, 2005).
The leaders in a hospital can adopt a questioning style which is more like discussion and certainly different from blaming (Vogus et al., 2020). University of Michigan Heath System (UMHS) initiated and implemented a program of complete openness replete with full disclosure and discovered that their patients had good experience and there wasn’t any increase in the liabilities or total claims. So, the practice of transparency by a healthcare institution ensured not only good experience but patient satisfaction too.
Hence, Transparency is one of the main dimensions specified and considered.
Research Gap: The literature is inconclusive about relationship amongst patient experience, patient satisfaction and quality of healthcare (Zakkar, 2019). Hence it has been subjected to interpretations of research scholars, healthcare providers and healthcare managers (Jerant et al., 2018; Zinckernagel et al., 2017). Also, different stakeholders of the healthcare have different expectations and varied perspectives about patient experience (Zakkar, 2019), thus there is no consensus on factors that create ideal patient experience (Panchapakesan et al., 2015).
In the extant review, various dimensions impacting the patient experience have been identified by previous researchers, but no one focused on ranking the dimensions. Studies on patient experience in Indian healthcare (Rohini & Mahadevappa, 2006; Duggirala et al., 2008; Naidu, 2009; Chakraborty & Mazumdaar, 2011; Chatterji & Srinivasan, 2013; Fatma, 2014; Padma & Wagenseil, 2016) have focused on overall quality improvement but not on patient experience as a factor.
1. There is no description of organizational factors alone (or in isolation), impacting the patient experience.
2. Ranking of factors in terms of their impact on the patient experience could not be found.
3. The difference in perceptions of patients in India compared to other developed economies have also not been recorded anywhere.
4. The importance of transparency being practiced at an organizational level and its impact on patient experience could not be found by the researcher.
Lee-Kong-Ghista (2006) confirms that a healthcare organization and its culture is a crucial factor, not only in understanding the ability of any organization to perform but also to compete. Hence, we wanted to isolate organizational factors and then study its effect on patient experience. To address the abovementioned gaps, this study delves deeper through a qualitative approach and answers the following questions.
1. RQ 1: What dimensions from organizational perspective create value and contribute to patient’s experience, in India? Are they different when compared to healthcare in developed world?
2. RQ 2: How do patients rank the organizational dimensions in the order of priority?
3. RQ 3: In India, how significant is the impact of organizational transparency on patient experience?
Methodology
In this paper, we have attempted to identify organizational factors that contribute to patient experience, in Indian context, using qualitative method of Netnography and manual coding.
We deployed Kozinet’s five step research protocol (Entrée, Data collection, Analysis & Interpretation, Ethics and Member Checks) to identify and classify the dimensions thus ensuring an adequate adaptation of ethnographic study. A three-stage coding, viz. Open coding, Axial coding, and Categorical coding was used for identification of grounded theory (Strauss & Corbin, 1998). Line by‐line and word‐by‐word analysis helped in identification of concepts from the phenomenon. Our methodology is close to non-participative observation approach.
Netnography is a relatively new method designed to provide consumer insights from social media data (Kozinets, 1998; Belk & Kozinet, 2005). It is used to collect primary data such as comments, discussions from online communities like Facebook, Twitter, LinkedIn, Youtube, Instagram etc. The views of supporters or user groups are formed on social media for a particular cause.
Ground Theory Approach and Netnography
The combination has often been used to develop the framework as an attempt to build theory and subjected to further empirical tests, validation, wherever possible.
Patient Experience and Social Media
Patient experience narrated on a social media platform becomes visible to large masses. Consumers planning to avail a particular service, these days, prefer to check it out on social networking sites. Such platforms are transforming the communication patterns and user groups are becoming highly interactive thus defining a new social phenomenon (Izogo & Jayawardhena, 2018; Verma, 2015).
Online Health Communities (OHC)
Zhao et al., 2015 talked about how the western world has seen emergence of online health communities (OHC)—a type of online social network where members interact. The advantage of such a group is to seek information and interact amongst the in health- or wellness-related virtual communities. These sites further assist in providing help, emotional support, and communication opportunities (Josefsson, 2005; Krcmar et al., 2002; Zhao et al., 2013). Patient’s opinions and idea exchanges contain rich medical and experiential knowledge (Zhao et al., 2013) and enable patients to access useful information.
Population and Sampling
The population considered was patients (or their relatives/attendants) who were hospitalized in the recent past and posted their experiences on websites which aggregates opinions during the visit to hospitals. The researcher also considered opinion aggregators which spans across bloggers and invites them to share their experiences. Nowadays even the healthcare bodies are very keen to know the experiences of their stake holders and allot space on their website seeking feedbacks. The advantage of independent narratives on the internet is unobtrusive in nature.
Data Collection and Platforms
Following Kozinet’s Entrée criteria, to identify appropriate online community, the researcher started with Google search engine to identify the best rated hospitals in Mumbai and its suburban areas. Amongst the websites like medifee.com, essencz.com, treatmenttraveller.com etc., the most popular one with lots of followers was clinicspots.com.
Hospitals were defined as the health care institution that provides patient treatment having more than 200 bed capacity, with specialized equipment and methodical staff. For qualitative study, top 25 hospitals in Mumbai were considered first and then shortlisted 12 hospitals based on size, speciality, number of reviews garnered etc (Verhoef et al., 2009)
Upon visiting the websites of respective hospitals and their pages on social media like Facebook and Twitter handles etc, we observed that most of the content was focusing on promoting their brand and relatively less on patient’s comments and complaints.
Mouthshut was one website where millions of unbiased and open comments/posts were being captured. The quality of posts/ data was found to be rational because the website aggregated both good and bad posts, with more than 700 Million plus users. Hence, we relied on this rich quality data. Based on these posts, the website also rated the hospitals on a scale of 5 by evaluating their medical services, infrastructure, and staff attitude where most of the experiences are co-created.
Sample Screening
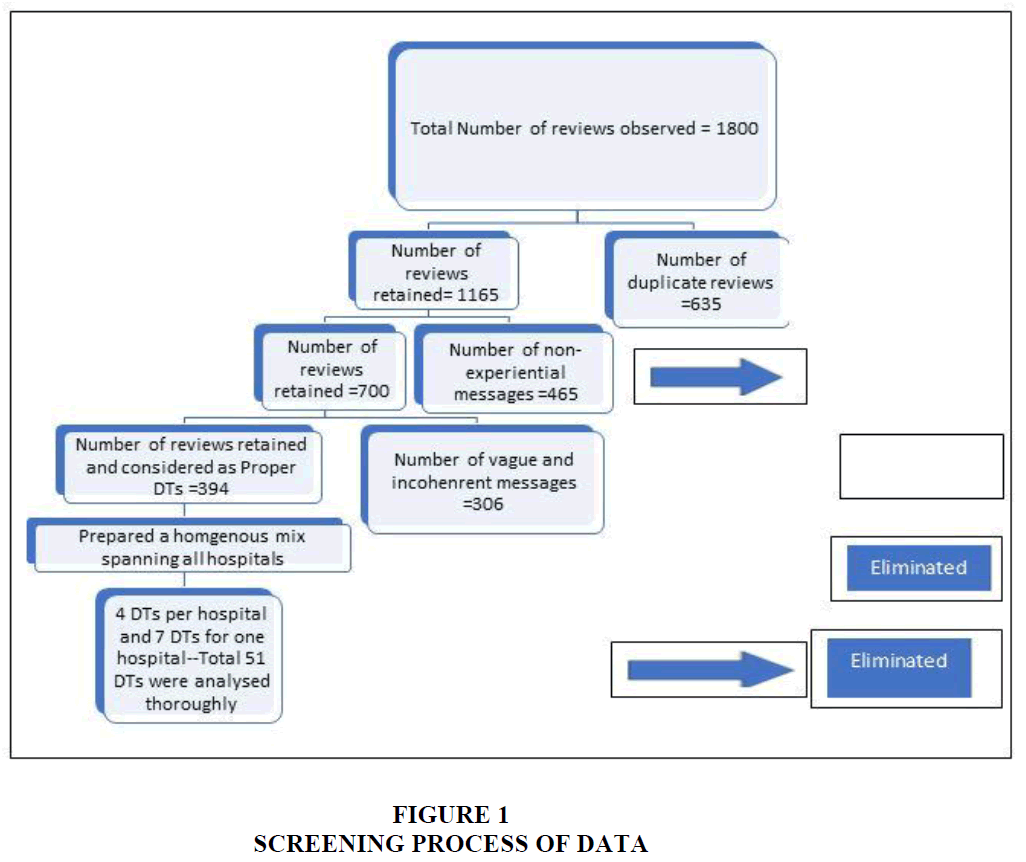
The comments were collated, studied, and then subjected to a rigorous review, in line with Kozinet’s stipulation of “Trustworthy Interpretations”. See (figure 1) describing the screening process. Comments providing dates, details of the incidences and referrals have been taken into consideration. Using this multiple iterative process, the number of data points were reduced to manageable limit and hence the total number of data points shortlisted were three hundred ninety-four. To maintain the homogeneity and representation of all twelve hospitals in a proportionate manner, qualitative data points for each hospital were limited to four except one hospital where seven posts were captured. Thus, the final number of discussion threads analysed was fifty-one (4x 11+7=51).
The process of screening the inputs is described in (Figure 1).
A snapshot of the hospitals shortlisted for the study is given in (Table 2) and the selection criteria of OPD, IPD and 200 beds capacity has already been described. To capture contrasting views and some focused homogeneity, the researcher included a government funded hospital and a super specialty CANCER hospital.
| Table 2 Snapshot of Selected Hospitals | |||||||
| S. No | Hospital Code | #of comments | Rating | IPD/OPD | # of Beds | Funding | Speciality |
| 1 | H3 | 57 | 2.98 | Both | 323 | Private | Multi-Sp |
| 2 | H4 | 6 | 2.17 | Both | 400 | Private | Multi-Sp |
| 3 | H5 | 59 | 1.71 | Both | 750 | Private | Multi-Sp |
| 4 | H6 | 71 | 2.75 | Both | 240 | Private | Multi-Sp |
| 5 | H9 | 25 | 2.48 | Both | 253 | Private | Multi-Sp |
| 6 | H10 | 17 | 2.29 | Both | 300 | Private | Multi-Sp |
| 7 | H15 | 26 | 3.12 | Both | 1800 | Government | Multi-Sp |
| 8 | H16 | 64 | 1.97 | Both | 1500 | Private | Multi-Sp |
| 9 | H18 | 10 | 2.3 | Both | 350 | Private | Multi-Sp |
| 10 | H19 | 5 | 3.2 | Both | 210 | Private | Multi-Sp |
| 11 | H20 | 18 | 2.13 | Both | 300 | Private | Multi-Sp |
| 12 | H22 | 36 | 3.22 | Both | 600 | Private | Cancer |
| Total | 394 | ||||||
Data Coding and Analysis
Upon identifying the posts describing the dates, persons involved and vivid description of experience, four comments per hospital were shortlisted to embark upon the coding process. Posts from these sources were captured and manual coding was applied. Initially, data was analysed for open codes by reviewing line‐by‐line analysis and constant comparison method. A three-stage coding, viz. Open coding, Axial coding, and Categorical coding was used for identification of grounded theory (Strauss & Corbin, 1998). Word‐by‐word analysis helped in identification of concepts from the phenomenon. Emergent concepts from open coding were classified and sorted into different buckets based on similarity and inferences (axial coding). Emergent categories (themes) were mapped for interrelationship. Finally, selective coding (Categorical) is used for finalization of emergent theory (grounded theory) based on theoretical saturation.
Findings and Discussion
Any institution can be built with marvellous infrastructure, backed up with world-class equipment and providing wonderful facilities but if the process orientation and systematic approach does not match up to patient’s (patients or companions) expectations, the reputation of the institution would certainly fall thus emphasizing the importance of organization’s role in value creation.
Billing, infrastructure, and associated systems/processes were of major concern for the patients and their companions. Check-out processes in the hospitals have been described as long and torturous, sometimes the procedure extending to many hours. Other points of concern alluded to attitude of doctors, staff, infrastructure, pricing, billing counter, information desk, systems approach, processes orientation, ethics, emotions, empathy, transparency, capabilities, brand, premises, tangibles like diagnostic labs, ambience, schedules, and services etc. However, in this paper our focus is confined to organizational factors only.
The researcher analysed the discussion threads by breaking them down into Open codes, Axial codes, and Categorical codes for grounded analysis. The researcher went through the words of posts captured to identify open codes with relevant concepts. Axial codes were contextualized with relevant portions of extant literature. Further categorization of axial codes was used to categorize and theorization. The description and illustration of Open codes, Axial codes and Categorical codes is presented in (Tables 3 and 4). We have not done any grammatical corrections/modifications to the Discussion Threads (DTs) to retain their originality. Sometimes, we have shortened the DT wherever repetitive narrations were indulged.
| Table 3 Discussion Threads and Coding | ||
| Illustrative Discussion Threads | Open Codes | Axial Codes |
| This hospital and the doctors and staff work for greed as they want their treated patients back as per their commercial purpose they don't treat their patients as patients but as a source of money. not reliable or recommendable. | Want patient back Not reliable or reccomendable |
System and Process Outcome |
| Hospital has got the worst staff in this world, the doctors are so irresponsible that they don't care about patients at all, no follow up at all between doctors, I don't understand how did they got job here. Highly unprofessional. | No follow up Unprofessional |
System and Process |
| On waiting we realised almost everyone who came in had incorrect schedules and the staff were adamant it was the patients fault and not thrir systems. You service is bullshit and for what you guys charge definitely not worth our time. | Incorrect Schedules Waste of time |
System and Process Outcome |
| I had heard about it's best medical facilities and surgical operations from my friends, but it was really true said by them……..Cleanliness is very nice. If you want best medical facility then this hospital is correct place. | Cleanliness, Best Medical Facility Correct Place |
Tangibles Outcome |
| Doctors never answered to the relatives of the patient thoroughly or politely. They always took everyone for granted. Cost and rates: I thought the prices would be according to the services of the hospital but it was not the case because the price of the general ward was too high | Never Answered High Pricing beyond expectation |
Transparency Pricing / Outcome |
| Table 4 Classification of Codes | ||
| Open Codes | Axial Code | CCategorical Code |
| No Clear communication, Genuine, Details not given, Reasons given, Expectations setting/not meeting, Timely Information, Cheating, Unnecessary tests/procedures, Cover-up processes, Excessive Billing, Unwillingness on Doctor’s part. | Transparency | Value Creation through Organization |
| P Poor processes, Confused Staff, Insensitive ops, (Un)Professional, Lack of processes, Coordination amongst departments/staff, Teamwork, good (or bad) service attitude, Going extra mile, proper medication, blotched ops/steps, refusal to attend/listen, disregard for rules, insensitiveness to emergency, partial attention, improper workload, diagnosis steps, Cashless handlings Ontime medication, coordination amongst doctors and staff, taking feedback, wanting patient back, switching doctors, unwarranted post, bad treatment, Money minded approach, Unsystematic. | system and Process | |
| Fa Facility, good (or inadequate) labs, cafeteria, Inadequate pharma, Ventilation, providing accessories, cleanliness, dirty, hygienic ambience, class of equipment, infrastructure. | Tangibles | |
| SuSuccessful, (Not) Recommended, satisfied, looting money, will come back, Encourage/Discourage others, excellent treatment. | Out comes | Out come |
Discussion on Codes
Although, the qualitative study supported most of the points emerged in the extant review of literature, few new findings emerged, especially in Indian context. First, amongst the hospitals in Mumbai, Safety was neither articulated nor any concern was shown, in any of the DTs perused. Second, it emerged that there were lots of patients willing to pay more for commensurate level of service and facilities, which is contrary to general belief that Indians consumers are ONLY price sensitive.
Amongst the 51 codes we analyzed, we could classify them into 5 Axial codes. Out of which 4 codes could be clubbed as Value creation by an organization and Outcomes.
The frequency of each of the axial code used has helped us to arrive at ranking and comprehend the order of priority. Details have been shown with respective frequency in (Table 5).
| Table 5 Axial Codes Value Creation (Organization) & Expereince and Ranking by Frequency | ||
| S. No | Axial Codes | Frequency of posts (Out of 51) |
| 1 | System and Process | 40 |
| 2 | Outcome | 29 |
| 3 | Trustworthiness or Transparency | 24 |
| 4 | Tangibles | 23 |
From the above data, we could see that majority of the patients are predominantly happy or unhappy with the System and Process - which is very much in the realms and controllable factor of an organization. Outcome, Transparency and Tangibles were the other criteria prevailing in the process of co-creation of experience.
We are reproducing some of the discussion threads shown below which corroborate the intent and perceptions of patients or their companions in each of the dimension identified. Since the discussion threads have been reproduced ad-verbatim, few grammatical errors and language flow may not be found appropriate.
System and Process (SP) was the pivotal point for patients or their companions to experience comfort or discomfort. The major points were to deal with were professionalism being exhibited, priorities being ranked, schedules being adhered to, time taken during admission or discharging, billing practices, audit, and accounting processes etc. Andaleeb, (1998) emphasize that hospitals not delivering patient satisfaction may be facing the chances of extinction. It is important that the patient must feel assured about being in capable hands. (Parasuraman et al., 1985). The competence while delivering the service and following the processes contribute to patient assurance.
1. Dt1 (sp)-hospital is full of patient and their attenders. Hospital security is very tight, and they search each and every person from below to top. before going there, we call and ask him. for appointment of .... And they give us date of appointment. We go there on the date but the doctor is not come due to some reason but hospital staff satisfied us with the junior resident dr and give us the date of surgery…... hospital and staff is good but they charge very high.- positive experience
2. DT2(SP)-We had booked and confirmed ( twice by phone) our appointment at 11.30 am with Dr, however on reaching there the receptionist told us that the appointment was at 1 pm, we told them it was confirmed yet they told u it was our fault. On waiting we realised almost everyone who came in had incorrect schedules and the staff were adamant it was the patients fault and not thrir systems -Negative Experience.
3. DT3(SP)My father's surgery was done very nicely ...I can say that Docter is very nice person..treated very genuenly with full attention...Docter is very amazing-Positive Experience
4. dt4(sp) suggested for an "emergency" admission in the same hospital & suggested for "emergency" coronary artery bypass surgery(cabg) to be performed… emergency is understood, but twice you reschedule a major surgery just because you have another emergencies. in spite of the fact that the patient was admitted under an emergency. what the hell are you saying guys. you are hopeless- negative experience
Transparency (TN). Often the patients find themselves at large without any clue as to what is happening next. The hapless persons are never informed about the plans, steps involved in a treatment, the possible repercussions, estimated costs. The strong belief that is permeating is that once someone gets into the clutches of a doctor or a hospital, your status is reduced to a helpless bystander. On the other hand, there are few incidences where the very fact that transparency was exhibited at every step, the recovery of patients was quite swift. The following two discussion threads show and corroborate our inference.
1. DT1(TN)Doctor say us that our patient will discharge in 7 day but he discharge us after 17 days..Negative Experience.
2. DT2(TN)-Unfortunately.. was admitted in this hospital ...close to my residence.... Big Name but a total waste of name… they are misusing the name. Blank Receptionist......Attitude of Doctors....never answered to the relatives of the patient thoroughly or politely... took everyone for granted. Negative Experience.
3. DT3(TN)-to get him checked up ..was seriously injured ..lost a lot of blood but the injury was still very serious but the doctors and the environment there and the extremely postive vibes in there made him forget that he was even injured… they were so comforting with patient and even spoke to us about the treatment in detail.- Positive Experience.
Tangibles (TG) like infrastructure, equipment, room facilities, associated para-medical services like pharmacy, Cafeterias etc. are perceived to be an important factor in selecting a hospital. Many patients feel that tangibles were not commensurate with the money being charged. The following two discussion thread would help in getting the intent.
1. DT(TG)-1-- service was prompt response. Doctor on duty reacted fast, attended promptly and medication given…..the ward is infested with mosquitos as doors are left open most of the time….Negative Experience.
2. DT(TG)-2-- The attitude of staff sucks like its free facility where u pay for 5 star service. Most of the services are crazily overcharged and are not worth it. Bad service initiation... Had to bring blanket ..didn't got time to give her a blanket or pillow till 6 hours after.. Negative Experience.
Outcome (OC) – The resultant experience garnered at various touchpoints can be called an outcome. Usually the outcome deals with satisfaction, delight (higher order of satisfaction), recommendations to other (positive or negative) and most importantly the willingness to come back (Retention). The following 2 DTs give us a flavor of Outcomes.
1. DT1(OC)At the time of discharge we paid a very high price for which the hospital was not worth of. Overall experience...My experience with the hospital is very poor, I will suggest to look for any other private hospital
2. DT2(OC)….has also great hospitality and care taking staff. Cleanliness is very nice. If you want best medical facility, then this hospital is correct place.
Implications
Our study contributes in many ways in understanding Patient Experience and the factors that drive it. Various stakeholders in healthcare system interpret patient experience in different ways owing to factors like patient’s condition, patient engagement, patient centricity, patient’s expectations (Zakkar, 2019), we stayed focused on Organizational factors that impact patient experience.
Our finding is that from an organizational perspective amongst Indian healthcare providers, the value creation is achieved by:
1. System and Process – System/order/approach/priorities while handling patients including proficiency in discharging the professional duties.
2. Outcome – Final take away of the patient.
3. Transparency - Gaining the trust through transparent practices.
4. Tangibles – Physical surroundings, building infrastructure, housekeeping, labs, cafeteria.
While patients in developed economies like USA/UK etc. experience these attributes in a definitive manner while rating the healthcare provider and prompt actions are taken to appease the patient or at least a rejoinder is often given, whereas in India, the response from healthcare provider is tepid and laced with recalcitrant attitude. No DT was found where any healthcare provider considered giving refunds or at least offered a note of apology.
Also, from the frequency of these factors, they are ranked in the order (See Table 1.5 for frequency) of System and Process, Outcomes, Transparency and Tangibles respectively.
System and Process was the most important dimension amongst the patients because one of the first impressions is with the immediate care and admission formalities of any hospital. Once the patient is addressed and admitted, then the proficiency of other services starts adding to their experience. This comes into reckoning for a patient after being exposed to systems and processes. With processes of an institution and gaining confidence on the proficiency of services, the patient starts forming opinions with small outcomes or events that would eventually lead them to satisfaction or otherwise.
Transparency as an organizational dimension in value creation has been reckoned relatively lower amongst patients in India compared to system and process. In the study, researcher observed multiple instances where the hospitals did not give any estimates of the proposed line of treatment and in some cases, even if the estimate was given, the final bills and expenses far exceeded the initial estimates. In India, where the choice of hospitals is mostly driven by the recommendation of treating physician, transparency takes a back seat when compared to other dimensions.
Tangibles were relatively low ranked in our study. General perception is that along with good infrastructure, any healthcare institution would have good equipment and testing facilities (Andaleeb, 1998; Lim & Tang, 2000; Naidu, 2009). This may not be true in India because a good number of hospitals still prefer to outsource diagnostic tests. Kathy Torpie (2014) mentioned that healthcare institutes that boast of a 5-star resort like facilities is raising the expectations which in turn is fueling the maintenance cost thus rendering the business unsustainable and unviable and this became apparent in our study, from some of the analyzed DTs.
Out of the analysed DTs, majority were talking about bad experiences compared to good experience. People were miffed about instances where they felt that hospitals were more focussed as a commercial organization rather than a service-oriented institution. The feeling that despite paying high prices, the quality of service was found to be much below their expectations.
Theoretical Implications
We have classified the factors that create value from an organizational perspective and contribute to patient experience. Our proposed classification scheme and ranking order would assist the researchers, in planning as well as delving deeper into any of the dimension while evaluating patient experience in any healthcare institution.
That is why mining hash-rate is vital. The more hashing power means the network is more secure. The hashing power of Bitcoin is still uncertain. However, it can be calculated based on the mined blocks and the blockchain difficulty.
Managerial Implications
Transparency (Trust) is one such dimension, which emerges as a distinct factor even in developing economy like India. The researcher feels that transparency could also be used as a marketing tool to instill confidence to consumers and transparency should be one of the prime prerogatives of institutions to impart faith into the minds of a consumer.
Our findings have practical implications in enhancing the reputation of a hospital. It can greatly assist managers in understanding how their patients assess the hospitals. Creating a unifying framework, with the identified factors here-in, it is possible for the hospital authorities to drive patient experience culminating into satisfaction and encouraging word of mouth to bring in referrals.
Given these findings, it is possible for the promoters as well as professionals running the hospitals to take cognizance of these explanatory dimensions, which can be readily acted on and incorporated in a hospital’s strategic stance. Embarking on a journey to monitor these dimensions which will ensure positive co-creation of experience with outcomes like delight and retention.
Limitations and Future Research Directions
A quantitative analysis with adequate sample size can be done to ratify the findings of our study. The inputs gathered from Netnography cannot be extrapolated to real life scenario and hence other qualitative techniques like triangulation can be deployed with various stakeholders to get a clear and lucid picture.
Conclusion
A quantitative study using established scales like SERVQUAL or NPS or EXQ can also be used to rank the hospitals in identified constructs like Process orientation, Transparency or Tangibles etc. This study was confined to hospitals based out of Mumbai in western zone of India. More number of hospitals covering other zones can be considered for future studies. This study was conducted by collating the comments in English language whereas similar approach can be extended to comments made in vernacular.
References
Alam, S., Osama, M., Iqbal, F., & Sawar, I. (2018). Reducing pharmacy patient waiting time. International Journal of Health Care Quality Assurance.
Indexed at, Google Scholar, Cross ref
Andaleeb, S.S. (1998). Determinants of customer satisfaction with hospitals: A managerial model. International Journal of Health Care Quality Assurance.
Indexed at, Google Scholar, Cross ref
Becker, E.R., & Steinwald, B. (1981). Determinants of hospital casemix complexity. Health Services Research, 16(4), 439.
Indexed at, Google Scholar, Cross ref
Belk, R.W., & Kozinets, R.V. (2005). Videography in marketing and consumer research. Qualitative Market Research: An international journal, 8(2), 128-141.
Indexed at, Google Scholar, Cross ref
Berry, L. L., & Carbone, L. P. (2007). Build loyalty through experience management. Quality Progress, 40(9), 26-32.
Boakye, K.G., Qin, H., Blankson, C., Hanna, M.D., & Prybutok, V.R. (2021). Operations-oriented strategies and patient satisfaction: the mediating effect of service experience. International Journal of Quality and Service Sciences.
Indexed at, Google Scholar, Cross ref
Brady, M.K., & Cronin Jr,J.J. (2001). Some new thoughts on conceptualizing perceived service quality: A hierarchical approach. Journal of Marketing, 65(3), 34-49.
Indexed at, Google Scholar, Cross ref
Chahal, H., Sharma, R.D., & Gupta, M. (2004). Patient satisfaction in public outpatient health care services. Journal of Health Management, 6(1), 23-45.
Indexed at, Google Scholar, Cross ref
Chahal, H., & Mehta, S. (2010). Antecedents and consequences of organisational citizenship behaviour (OCB): A conceptual framework in reference to health care sector. Journal of Services Research, 10(2), 25.
Chakraborty, R., & Majumdar, A. (2011). Measuring consumer satisfaction in health care sector: The applicability of servqual. Researchers World, 2(4), 149.
Deloitte, I. (2017). Predicciones sobre tecnología, medios y telecomunicaciones: https://www2. deloitte. com/content/dam/Deloitte/cr/Documents/technology-media-telecommunications/estudios. TMT-Predictions-2017-spanish. pdf.
Duggirala, M., Rajendran, C., & Anantharaman, R.N. (2008). Patient‐perceived dimensions of total quality service in healthcare. Benchmarking: An international journal.
Indexed at, Google Scholar, Cross ref
Ellison, A. (2015). Geisinger to begin offering refunds to unsatisfied patients. Becker’s Hospital Review. Available at: http:// www.beckershospitalreview.com/finance/geisinger-to-beginoffering- refunds-to-unsatisfied-patients.html.
Fatma, S. (2014). Antecedents and consequences of customer experience management-a literature review and research agenda. International Journal of Business and Commerce, 3(6).
Ferrand, Y.B., Siemens, J., Weathers, D., Fredendall, L.D., Choi, Y., Pirrallo, R.G., & Bitner, M. (2016). Patient satisfaction with healthcare services a critical review. Quality Management Journal, 23(4), 6-22.
Indexed at, Google Scholar, Cross ref
Gualandi, R., Masella, C., & Tartaglini, D. (2019). Improving hospital patient flow: A systematic review. Business Process Management Journal.
Indexed at, Google Scholar, Cross ref
Harris, K., Harris, R., & Baron, S. (2001). Customer participation in retail service: lessons from Brecht. International journal of Retail & Distribution Management.
Indexed at, Google Scholar, Cross ref
Iyer, V., Prissel, P., Munson, K., Eide, J., Brustad, R., Kranz, N., & Frase, B. (2018). How to build a robust provider improvement partnership program to enhance patient experience–A case study. Patient Experience Journal, 5(1), 126-136.
Indexed at, Google Scholar, Cross ref
Izogo, E.E., & Jayawardhena, C. (2018). Online shopping experience in an emerging e‐retailing market: Towards a conceptual model. Journal of Consumer Behaviour, 17(4), 379-392.
Indexed at, Google Scholar, Cross ref
Jerant, A., Fenton, J.J., Kravitz, R.L., Tancredi, D.J., Magnan, E., Bertakis, K.D., & Franks, P. (2018). Association of clinician denial of patient requests with patient satisfaction. JAMA internal medicine, 178(1), 85-91.
Indexed at, Google Scholar, Cross ref
Josefsson, U. (2005). Coping with illness online: The case of patients' online communities. The Information Society, 21(2), 133-141.
Indexed at, Google Scholar, Cross ref
Kozinets, R.V. (1998). On netnography: Initial reflections on consumer research investigations of cyberculture. ACR North American Advances.
Krcmar, H., Arnold, Y., Daum, M., & Leimeister, J.M. (2002). Virtual communities in health care: The case of" krebsgemeinschaft. de". ACM SIGGROUP Bulletin, 23(3), 18-23.
Indexed at, Google Scholar, Cross ref
Lee, P.M., Khong, P., & Ghista, D.N. (2006). Impact of deficient healthcare service quality. The TQM Magazine.
Indexed at, Google Scholar, Cross ref
Lim, P.C., & Tang, N.K. (2000). A study of patients’ expectations and satisfaction in Singapore hospitals. International Journal of Health Care Quality Assurance.
Indexed at, Google Scholar, Cross ref
Meesala, A., & Paul, J. (2018). Service quality consumer satisfaction and loyalty in hospitals: Thinking for the future. Journal of Retailing and Consumer Services, 40, 261-269.
Indexed at, Google Scholar, Cross ref
Naidu, A. (2009). Factors affecting patient satisfaction and healthcare quality. International Journal of Health Care Quality Assurance.
Indexed at, Google Scholar, Cross ref
Otani, K., Kurz, R.S., & Barney, S.M. (2004). The impact of nursing care and other healthcare attributes on hospitalized patient satisfaction and behavioral intentions. Journal of Healthcare Management, 49(3), 181.
Indexed at, Google Scholar, Cross ref
Padma, P., Rajendran, C., & Lokachari, P. S. (2010). Service quality and its impact on customer satisfaction in Indian hospitals. Benchmarking: An International Journal. 17(6), 807-84.
Indexed at, Google Scholar, Cross ref
Padma, P., & Wagenseil, U. (2016). Antecedents of Service Excellence. In 4 th International Conference on Contemporary Marketing Issues ICCMI June 22-24, 2016 Heraklion, Greece (454).
Panchapakesan, P., Sai, L. P., & Rajendran, C. (2015). Customer satisfaction in Indian hospitals: Moderators and mediators. Quality Management Journal, 22(1), 10-29.
Indexed at, Google Scholar, Cross ref
Parasuraman, A., Zeithaml, V. A., & Berry, L.L. (1985). A conceptual model of service quality and its implications for future research. Journal of Marketing, 49(4), 41-50.
Indexed at, Google Scholar, Cross ref
Press, I. (2006). Patient satisfaction: Understanding and managing the experience of care. Chicago: Health Administration Press.
Quigley, D.D., Mendel, P.J., Predmore, Z.S., Chen, A.Y., & Hays, R.D. (2015). Use of CAHPS® patient experience survey data as part of a patient-centered medical home quality improvement initiative. Journal of Healthcare Leadership, 7, 41.
Indexed at, Google Scholar, Cross ref
Rao, M., Clarke, A., Sanderson, C., & Hammersley, R. (2006). Patients' own assessments of quality of primary care compared with objective records based measures of technical quality of care: Cross sectional study. Bmj, 333(7557), 19.
Indexed at, Google Scholar, Cross ref
Rohini, R., & Mahadevappa, B. (2006). Service quality in Bangalore hospitals-an empirical study. Journal of Services Research, 6(1), 59.
Seedhouse, D. (2008). Ethics: the heart of health care. John Wiley & Sons.
Shabbir, A., Malik, S.A., & Malik, S.A. (2016). Measuring patients healthcare service quality perceptions, satisfaction, and loyalty in public and private sector hospitals in Pakistan. International Journal of Quality & Reliability Management.
Indexed at, Google Scholar, Cross ref
Sofaer, S., & Firminger, K. (2005). Patient perceptions of the quality of health services. Annu. Rev. Public Health, 26, 513-559.
Indexed at, Google Scholar, Cross ref
Stein, T., Frankel, R.M., & Krupat, E. (2005). Enhancing clinician communication skills in a large healthcare organization: A longitudinal case study. Patient Education and Counseling, 58(1), 4-12.
Indexed at, Google Scholar, Cross ref
Strauss, A., & Corbin, J. (1998). Basics of qualitative research techniques.
Studer, Q. (2003). How healthcare wins with consumers who want more. Frontiers of Health Services Management, 19(4), 3.
Indexed at, Google Scholar, Cross ref
Torpie, K. (2014). Customer service vs. Patient care. Patient Experience Journal, 1(2), 6-8.
Vandamme, R., & Leunis, J. (1993). Development of a multiple-item scale for measuring hospital service quality. International Journal of Service Industry Management, 4(3), 0-0.
Indexed at, Google Scholar, Cross ref
Verhoef, P. C., Lemon, K.N., Parasuraman, A., Roggeveen, A., Tsiros, M., & Schlesinger, L.A. (2009). Customer experience creation: Determinants, dynamics and management strategies. Journal of Retailing, 85(1), 31-41.
Indexed at, Google Scholar, Cross ref
Verma, S. (2015). Harnessing the benefit of social networking sites for intentional social action: Determinants and challenges. Vision, 19(2), 104-111.
Indexed at, Google Scholar, Cross ref
Vogus, T.J., & Mc Clelland, L.E. (2016). When the customer is the patient: Lessons from healthcare research on patient satisfaction and service quality ratings. Human Resource Management Review, 26(1), 37-49.
Indexed at, Google Scholar, Cross ref
Vogus, T. J., Gallan, A., Rathert, C., El-Manstrly, D., & Strong, A. (2020). Whose experience is it anyway? Toward a constructive engagement of tensions in patient-centered health care. Journal of Service Management.
Indexed at, Google Scholar, Cross ref
Worlu, R., Kehinde, O.J., & Borishade, T.T. (2016). Effective customer experience management in health-care sector of Nigeria: A conceptual model. International Journal of Pharmaceutical and Healthcare Marketing.
Indexed at, Google Scholar, Cross ref
Zakkar, M. (2019). Patient experience: Determinants and manifestations. International Journal of Health Governance.
Indexed at, Google Scholar, Cross ref
Zifko-Baliga, G.M., & Krampf, R.F. (1997). Managing perceptions of hospital quality. Marketing Health Services, 17(1), 28.
Zinckernagel, L., Schneekloth, N., Zwisler, A.D.O., Ersbøll, A.K., Rod, M.H., Jensen, P.D., & Holmberg, T. (2017). How to measure experiences of healthcare quality in Denmark among patients with heart disease? the development and psychometric evaluation of a patient-reported instrument. BMJ open, 7(10), e016234.
Indexed at, Google Scholar, Cross ref
Zhao, J., Ha, S., & Widdows, R. (2013). Building trusting relationships in online health communities. Cyberpsychology, Behavior, and Social Networking, 16(9), 650-657.
Indexed at, Google Scholar, Cross ref
Zhao, J., Wang, T., & Fan, X. (2015). Patient value co-creation in online health communities. Journal of Service Management. 26 (1).
Indexed at, Google Scholar, Cross ref
Received: 10-May-2022, Manuscript No. AMSJ-22-11907; Editor assigned: 11-May-2022, PreQC No. AMSJ-22-11907(PQ); Reviewed: 25-May-2022, QC No. AMSJ-22-11907; Revised: 27-May-2022, Manuscript No. AMSJ-22-11907(R); Published: 30-May-2022